Tubulointerstitial nephritis
Tubulointerstitial nephritis (TIN) or Tubulointerstitial diseases can be of two types- Primary and Secondary
Secondary tubulointerstitial disease: Inflammation or fibrosis of the renal interstitium and atrophy of the tubular compartment following the glomeruli or vascular diseases.
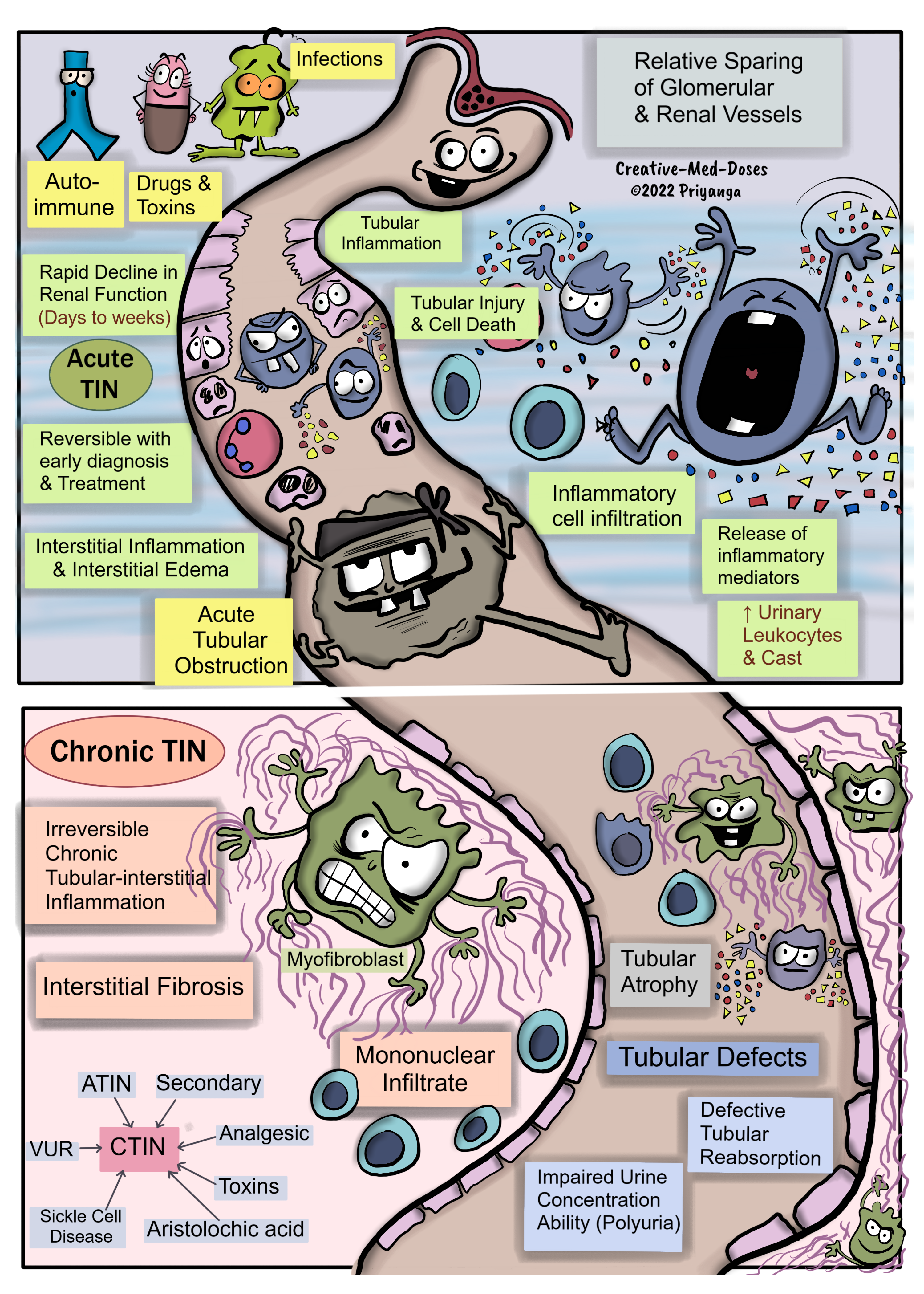
Primary Tubulointerstitial Nephritis (TIN)- primarily affects the tubules and interstitium, with relative sparing of the glomeruli and renal vessels. Glomerulus and renal vessels get involved in the later stages of the disease.
Primary Tubulointerstitial nephritis can be acute and chronic tubulointerstitial nephritis (TIN).
Acute Tubulointerstitial Nephritis (ATIN)-Tubulo-interstitial inflammation causes a rapid decline in renal function within days to weeks. It is reversible with early diagnosis and prompt treatment.
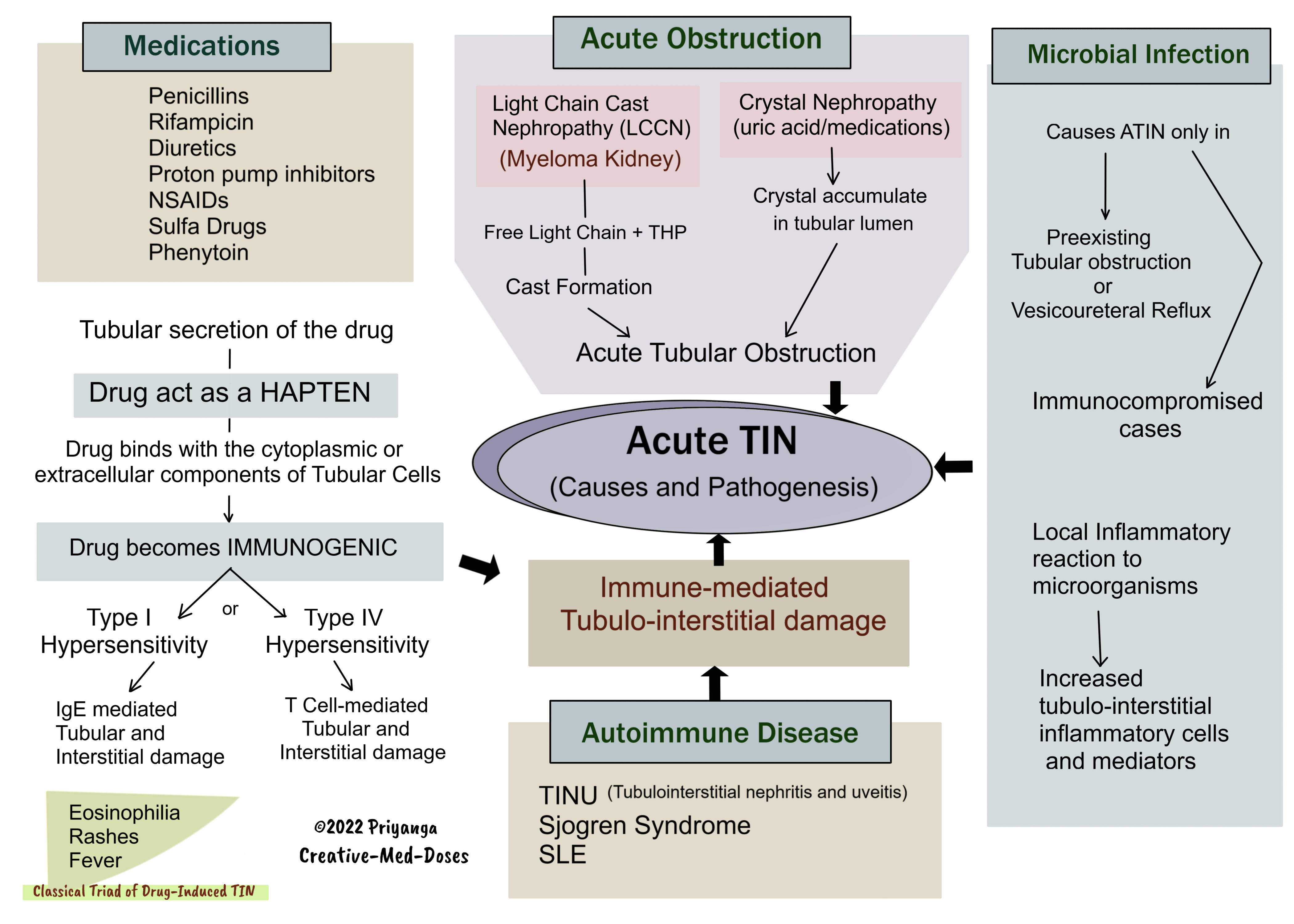
Causes and Pathogenesis of ATIN
Drug-induced TIN
Following drugs are the most common etiological factor of Drug-induced ATIN-
- Penicillin
- Rifampicin
- Diuretics
- Proton pump inhibitors
- NSAIDs
- Sulfa Drugs
- Phenytoin
Tubular secretion of the drug→ Drug act as a HAPTEN →Drug binds with the cytoplasmic or extracellular components of Tubular Cells →Drug becomes IMMUNOGENIC → Immune-mediated tubular-interstitial damage (Type I hypersensitivity or Type IV hypersensitivity).
Type I hypersensitivity
IgE mediated Tubular and Interstitial damage
Classical Triad of Drug-Induced TIN
- Eosinophilia
- Rashes
- Fever
Type IV hypersensitivity - T Cell-mediated Tubular and interstitial damage
Autoimmune Diseases
Autoantibodies and immune complexes lead to Immune-mediated tubular-interstitial damage.
Most common autoimmune diseases associated with Acute TIN-
- Tubulointerstitial Nephritis and Uveitis Syndrome (TINU)
- Sjogren Syndrome
- SLE
Acute Tubular Obstruction
Light Chain Cast Nephropathy (LCCN), also known as Myeloma Kidney/ Crystal Nephropathy (uric acid/medications) →Acute tubular obstruction →Tubular injury and inflammation → Tubulointerstitial nephritis and acute tubular necrosis if left untreated →Acute Renal Failure.
Microbial Infection
Microbial infection (bacteria/virus/fungi) → stimulates tubulointerstitial inflammation →Acute TIN.
The microbial infection causes ATIN only in Preexisting Tubular obstruction /Vesicoureteral Reflux or Immunocompromised cases.
Clinical Features -Depends on the underlying cause
Signs and symptoms of acute kidney injury
Classic triad (most commonly seen in drug-induced TIN)
- Eosinophilia
- Fever
- Rash
Flank pain
Arthralgias
Treatment of Acute TIN
- Remove nephrotoxins, eliminate drugs causing TIN
- Treat Underlying etiology
- Glucocorticoids in unresponsive cases (except TIN related to infection)
- Untreated Acute TIN may progress to Chronic TIN and cause end-stage renal disease needing renal replacement therapy.
....
....
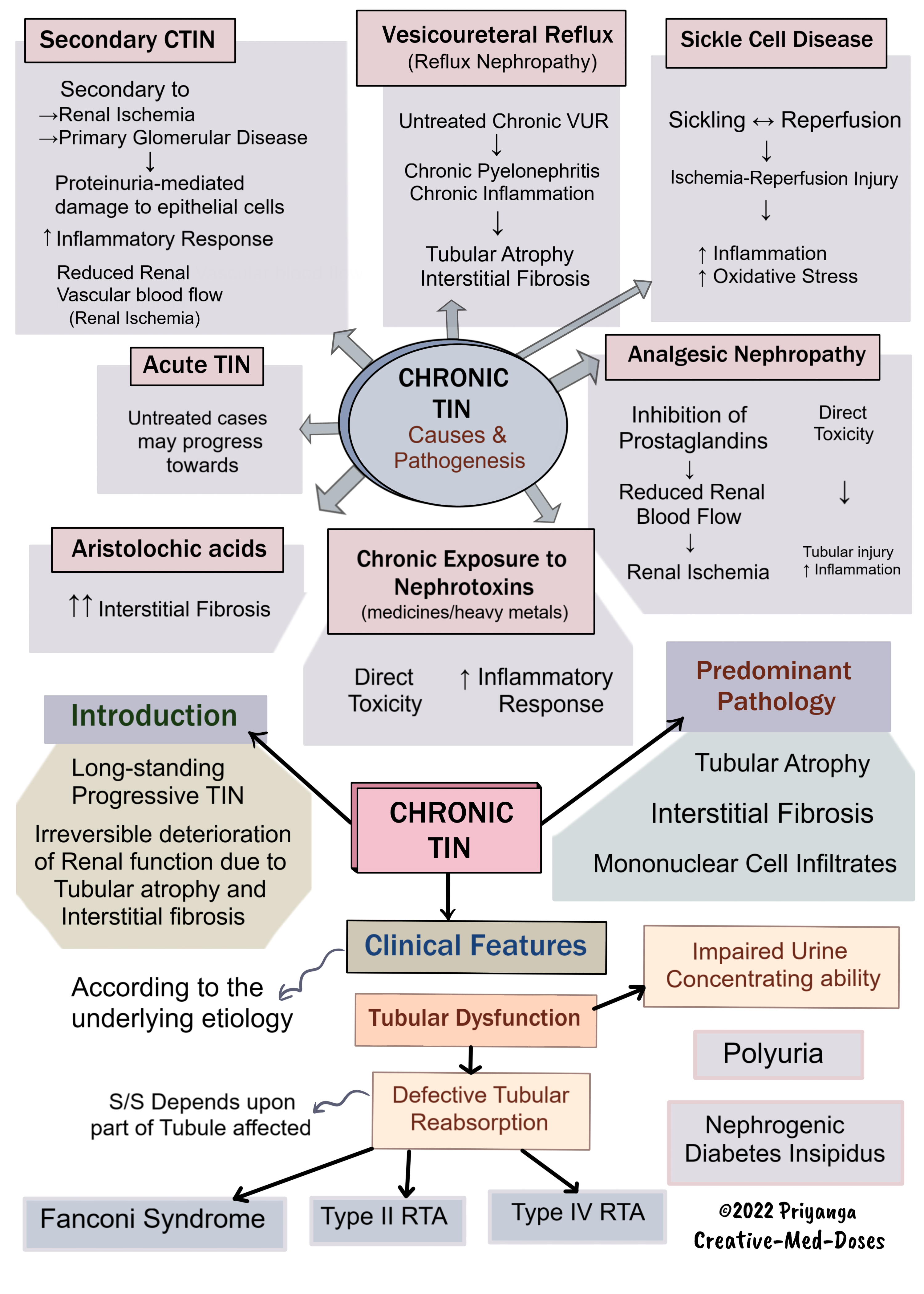
Chronic Tubulointerstitial Nephritis (CTIN)
Interstitial mononuclear cell infiltration → Chronic inflammation in tubules and interstitium → Tubular atrophy and interstitial fibrosis → Glomerulosclerosis and End stage renal disease (ESRD)
Predominant pathology – interstitial mononuclear infiltrates tubular atrophy and interstitial fibrosis.
Causes and Pathogenesis of CTIN
Secondary CTIN
Secondary CTIN following renal ischemia or primary glomerular diseases is the most common form of CTIN.
Mechanism of injury -
- Proteinuria-mediated damage to epithelial cells
- Inflammatory Response
- Reduced Renal Vascular blood flow (Renal Ischemia)
Following Acute TIN
Untreated ATIN may progress towards chronic form.
Analgesic nephropathy-
Inhibition of Prostaglandins→ Reduced Renal Blood Flow →Renal Ischemia
Direct Toxicity- Tubular injury and cell death
Chronic exposure to Nephrotoxins (medicines/heavy metals)
- Direct Toxicity to a nephrotoxin
- Inflammatory Response to nephrotoxins
Vesicoureteral Reflux (Reflux Nephropathy)
Untreated Chronic VUR→ Chronic Pyelonephritis & Chronic Inflammation →Tubular Atrophy & Interstitial Fibrosis
Sickle cell disease
Recurrent episodes of (Sickling ↔ Reperfusion) → Ischemia-Reperfusion Injury→ Inflammation and Oxidative Stress →Tubular Atrophy and interstitial fibrosis
Clinical features
- According to the underlying etiology
- Tubular Dysfunction
Defective Tubular Reabsorption - S/S Depends upon the part of the Tubule affected
- Fanconi Syndrome
- Type II RTA
- Type IV RTA
Impaired Urine Concentrating ability
- Polyuria (Nephrogenic Diabetes Insipidus)
Treatment - Treat the underlying cause and manage chronic kidney disease.
Revision for today Barrett’s esophagus - Creative Med Doses
Revision for today Renal Hypoxia: Why kidney is prone to hypoxia and ischemic injury? - Creative Med Doses
....
....
Buy fun review books here (these are Kindle eBooks you can download Kindle on any digital device and log in with an Amazon account to read them). Have fun and please leave a review.
https://creativemeddoses.com/books/
....
....