Henoch-Schonlein Purpura: IgA vasculitis
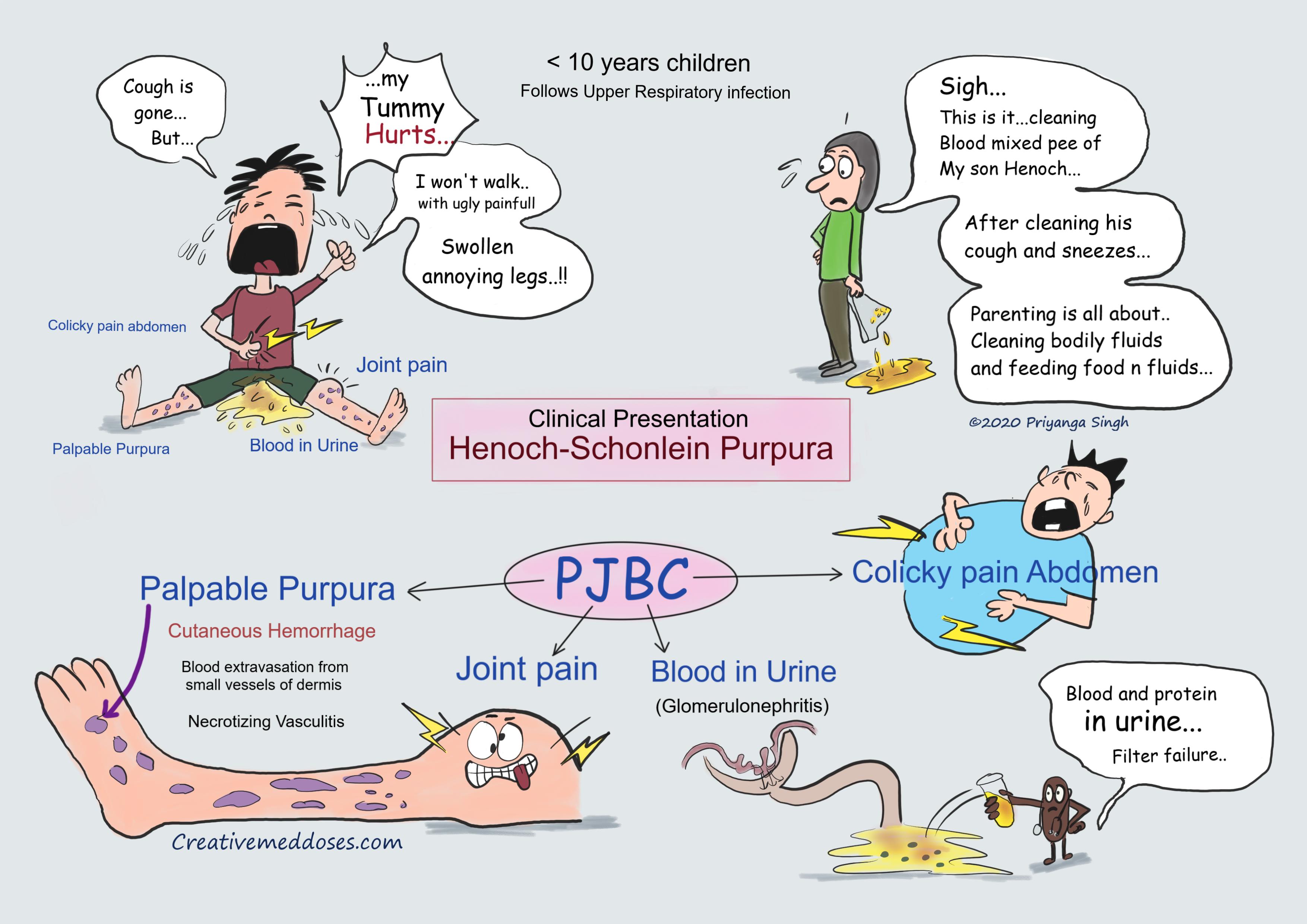
Henoch-Schonlein purpura (HSP) is also called IgA vasculitis, it is a small-vessel vasculitis characterized by palpable purpura, arthralgias, abdominal pain and hematuria.
It is most common childhood vasculitis and children < 10 years of age are most commonly affected.
It follows upper respiratory tract infection (especially with group A streptococcus or parvovirus B19). The child will have history of recent URI in most cases presenting with HSP.
Pathogenesis
The central pathogenic mechanism for Henoch-Schönlein purpura/ IgA vasculitis is immune-complex deposition. Henoch–Schönlein purpura is a small-vessel vasculitis in which complexes of immunoglobulin A (IgA) and complement component 3 (C3) are deposited on arterioles, capillaries, and venules. It is a type III hypersensitivity reaction.
Various infectious agents and Allergens, such as foods, horse serum, insect bites, exposure to cold, and drugs (e.g., ampicillin, erythromycin, penicillin, quinidine, and quinine), may work as antigen and stimulates IgA production.
HSP is a type of hypersensitivity vasculitis where inflammatory mediators such as Tumor necrosis factor (TNF), IL-1, and IL-6 may mediate the inflammatory process. Transforming growth factor (TGF)–β is a recognized stimulant of IgA production.
IgA plays a critical role in the immunopathogenesis of HSP. There are increased serum IgA concentrations, IgA-containing circulating immune complexes, and IgA deposition in vessel walls and renal mesangium of cases presenting with HSP.
IgA aggregates or IgA complexes with complement deposited in target organs, resulting in secretion of inflammatory mediators, including vascular prostaglandins such as prostacyclin, which plays a central role in the pathogenesis of HSP vasculitis.
Clinical features
PJBC are most frequently found sign and symptoms
Palpable purpura (small, raised areas of bleeding underneath the skin) with no thrombocytopenia. If the patient has thrombocytopenia diagnosis of HSP should be doubted. Palpable purpura is first to appear and is hallmark of HSP. Most common presenting symptom (95-100% of cases), especially involving the legs and dependent parts of body (like buttocks and thighs in children less than 3 years).
Joint pain (arthralgia)- The large joints (e.g., the knees and ankles) are the ones most involved, with pain and edema being the only symptoms.
Blood in urine (Hematuria)- 40-45 percent of cases has kidney involvement, mainly in the form of hematuria (blood in the urine) and proteinuria.
Renal involvement is characterized by mild glomerulonephritis resulting proteinuria and microscopic hematuria, with red blood cell casts in the majority of patients; it usually resolves spontaneously without therapy. In few cases progressive glomerulonephritis will develop which causes persistent hematuria and significant proteinuria leading to edema and significant protein deficiency.
Renal pathology is the most important cause of morbidity and mortality in patients with HSP.
Colicky abdominal pain – with nausea and vomiting is seen in most cases. It is frequently accompanied by the passage of blood and mucus per rectum and bowel intussusception may occur.
...
...
Diagnosis
The diagnosis of IgA vasculitis (Henoch-Schönlein) is based on clinical signs and symptoms. Most cases are clinically diagnosed.
- Blood test- normal platelet count normal blood picture.
- Urinalysis - proteinuria and hematuria indicates renal involvement.
- Skin biopsy – Histopathologic features of the skin lesions in infantile HSP can range from a typical leukocytoclastic vasculitis with or without fibrinoid necrosis to the less specific findings of a lymphohistiocytic perivascular infiltrate with extravasation of erythrocytes.
- Direct immunofluorescence (DIF)- It is a useful adjunct to histopathology IgA and C3 deposition can be detected by immunofluorescence.
- Renal biopsy – Renal biopsy is rarely needed for diagnosis but may provide prognostic information in some patients. The main findings on kidney biopsy are increased cells and Ig deposition in the mesangium (part of the glomerulus, where blood is filtered), white blood cells, and the development of crescents.
It should be performed when nephrotic syndrome persists and when renal function deteriorates. The extent of the crescents is of prognostic importance.
Treatment
Henoch-Schonlein Purpura/ IgA vasculitis has high spontaneous recovery rate. Most patients recover within 4-8 weeks without treatment.
Most cases without complication just need supportive care, like joint pain management and skin lesion treatment.
Supportive care – hydration and analgesics.
Persistent cases – rarely few patients develop persistent nephritis which has significant hematuria and proteinuria. These cases need following treatment –
- Corticosteroids
- Cytotoxic drugs- cyclophosphamide and Azathioprine
- Plasmapheresis
Prognosis
Most cases of Henoch-Schonlein Purpura/ IgA vasculitis have excellent prognosis with spontaneous recovery.
Following are main indicators for bad prognosis in most cases –
- Bloody stools
- Persistent rash
- Heavy proteinuria more than 3 months
Revision for today sideroblastic anemia.
Buy fun review books here (these are kindle eBook’s you can download kindle on any digital device and login with Amazon accounts to read them). Have fun and please leave review.
Subscribe YouTube channel here.
Case scenario
A 7-year-old boy presents to his pediatrician with a rash and intermittent abdominal pain. He also has knee joint pain, and ankle edema. Boy’s mother gave history of him Recovering from upper respiratory tract infection. On exam, the pediatrician noted dark purple, non-blanching papules and plaques that are distributed symmetrically over the patient's buttocks and legs. Blood test were normal, and urinalysis shows proteinuria. What is the underlying process causing this patient's dermatological findings?
A. Histamine release
B. Immune-mediated platelet destruction
C. IgA-mediated vasculitis
D. Anti-neutrophil cytoplasmic antibodies