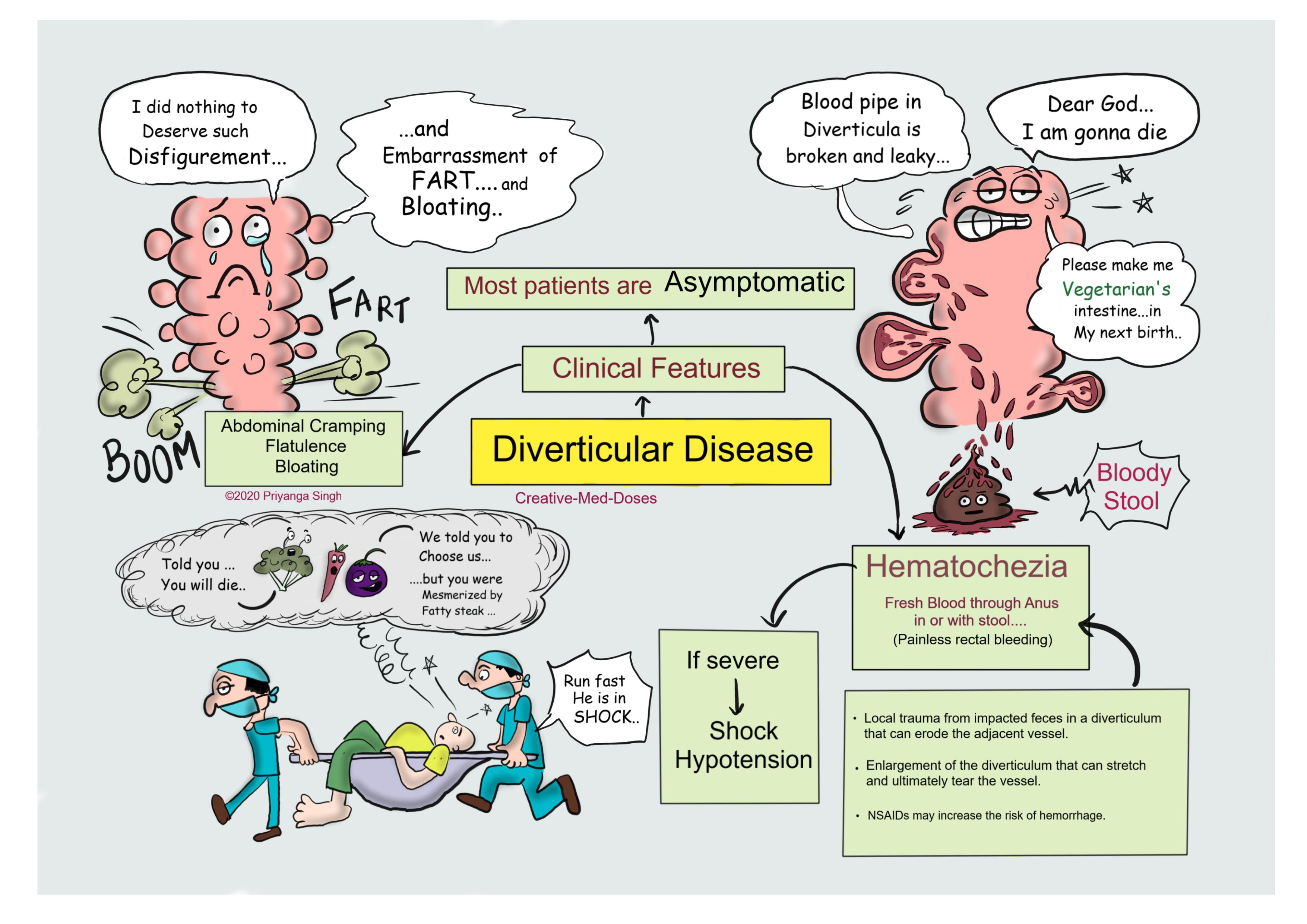
Diverticular disease of intestine
Diverticular disease has become the most common gastrointestinal disorder in the United States and is the leading indication for elective colon resection. The incidence of diverticular disease is on the rise.
Formerly, diverticular disease was confined to developed countries but with the adoption of westernized diets in underdeveloped countries, diverticulosis is on the rise across the globe.
Diverticular disease of GIT is the condition of having multiple sac-like protrusions (diverticula) of the colonic wall and can cause painless rectal bleeding.
Risk Factors
- Old age
- low dietary fiber
- high fat and red meat intake
- physical inactivity
- obesity
- smoking
- positive family history
- nonsteroidal anti-inflammatory drugs (NSAIDs)
Anatomy and Pathophysiology
Two types of diverticula occur in the intestine-
- True- A true diverticulum is a saclike herniation of the entire bowel wall
- False (pseudo diverticula)- pseudo diverticulum involves only a protrusion of the mucosa and submucosa through the muscularis propria of the colon. The type of diverticulum most commonly affecting the colon is the pseudo diverticulum.
The diverticula occur at the point where the nutrient artery, or vasa recti, penetrates through the muscularis propria, resulting in a break in the integrity of the colonic wall. This anatomic restriction may be a result of the relative high-pressure zone within the muscular sigmoid colon. Thus, higher-amplitude contractions combined with constipated, high-fat-content stool within the sigmoid lumen in an area of weakness in the colonic wall results in the creation of these diverticula. Consequently, the vasa recti are either compressed or eroded, leading to either perforation or bleeding.
Chronic low-grade inflammation is thought to play a key role in neuronal degeneration leading to dysmotility and high intraluminal pressure. Therefore, pockets or outpouchings develop in the colonic wall where it is weakest.
...
...
Clinical Symptoms of Diverticulum
- asymptomatic
- cramping
- bloating
- flatulence
- irregular defecation
- painless rectal bleeding--Hemorrhage from a colonic diverticulum is the most common cause of hematochezia in patients >60 years, yet only 20% of patients with diverticulosis will have gastrointestinal bleeding
- left lower quadrant (LLQ) pain and tenderness (because sigmoid colon is situated in LLQ, which is the most common site for diverticula.
Diagnosis
Colonoscopy is gold standard in diagnosing uncomplicated diverticula, but it is not recommended in inflamed diverticula.
Computed tomography (CT) with contrast is modality of choice in case of complicated diverticula such as diverticulitis and perforated diverticula.
Treatment
High-fiber diet to prevent constipation.
In case of diverticular bleeding –
If patient is stable-
- mesenteric angiography can localize the bleeding site, the vessel can be occluded successfully with a highly selective coil embolization.
- selective infusion of vasopressin
If patient is unstable- 6-unit bleed within 24 h
Surgery should be done
- If bleeding is localized – segmental resection can be performed
- If bleeding cannot be localized -- subtotal colectomy is done.
Diverticulitis with fever and Leukocytosis -is treated with Bowel rest (NPO) and IV antibiotics.
Perforated diverticulitis is treated by partial colectomy and anastomosis.
Revision for today https://creativemeddoses.com/topics-list/tetralogy-of-fallot-fatal-four/
Further reading https://emedicine.medscape.com/article/173388-overview#a6