Bronchiectasis
Bronchiectasis is an obstructive lung disease characterized by chronic necrotizing damage of smooth muscles and elastic support tissue of bronchi and bronchioles. It consequently leads to permanent irreversible dilation of bronchi and bronchioles. The involved bronchi and bronchioles are filled with excessive mucus and lead to reduced airflow. The bronchial dilation can be cylindrical (most common), varicose, or cystic.
The lung involvement can be focal or diffused.
- Focal - seen in tumor or foreign body impaction, bronchiectasis is localized to the obstructed lung segment.
- Diffused – seen in infection or immunodeficiency state, widespread bronchiectasis involving the entire lung.
Etiopathogenesis
Chronic necrotizing inflammation of the bronchi, caused by bronchial obstruction/ infection or impaired mucociliary clearance, is central to the pathogenesis of most cases of bronchiectasis.
Obstruction- bronchial obstruction due to tumor (internal/ external), lymphadenopathy, or foreign body
Infection – tuberculosis, staphylococcus aureus, pseudomonas aeruginosa
Impaired Mucociliary Clearance
Cystic fibrosis
Mutation in CFTR gene → Reduced chloride ion secretion in the mucus of respiratory epithelium → Thick and viscid mucus → Cilia cannot move smoothly in thick viscid mucus →Impaired Mucociliary clearance →Reduced removal of pathogens →Superimposed infection→ Chronic necrotizing inflammation → Bronchial wall damage → Permanent bronchial dilation → Bronchiectasis.
Please read more about Cystic Fibrosis - Creative Med Doses
Primary ciliary dyskinesia
Autosomal recessive mutation → Defect in motile cilia production or function → Immotile cilia is unable to sweep mucus → Impaired Mucociliary clearance→ Reduced removal of pathogens → Superimposed infection → Chronic necrotizing inflammation → Bronchial wall damage → Permanent bronchial dilation → Bronchiectasis.
Immotile cilia also lead to infertility and dextrocardia
Kartagener syndrome
- Situs inversus
- Chronic sinusitis
- Bronchiectasis
Read about Kartagener syndrome where cilia doesn't move - Creative Med Doses
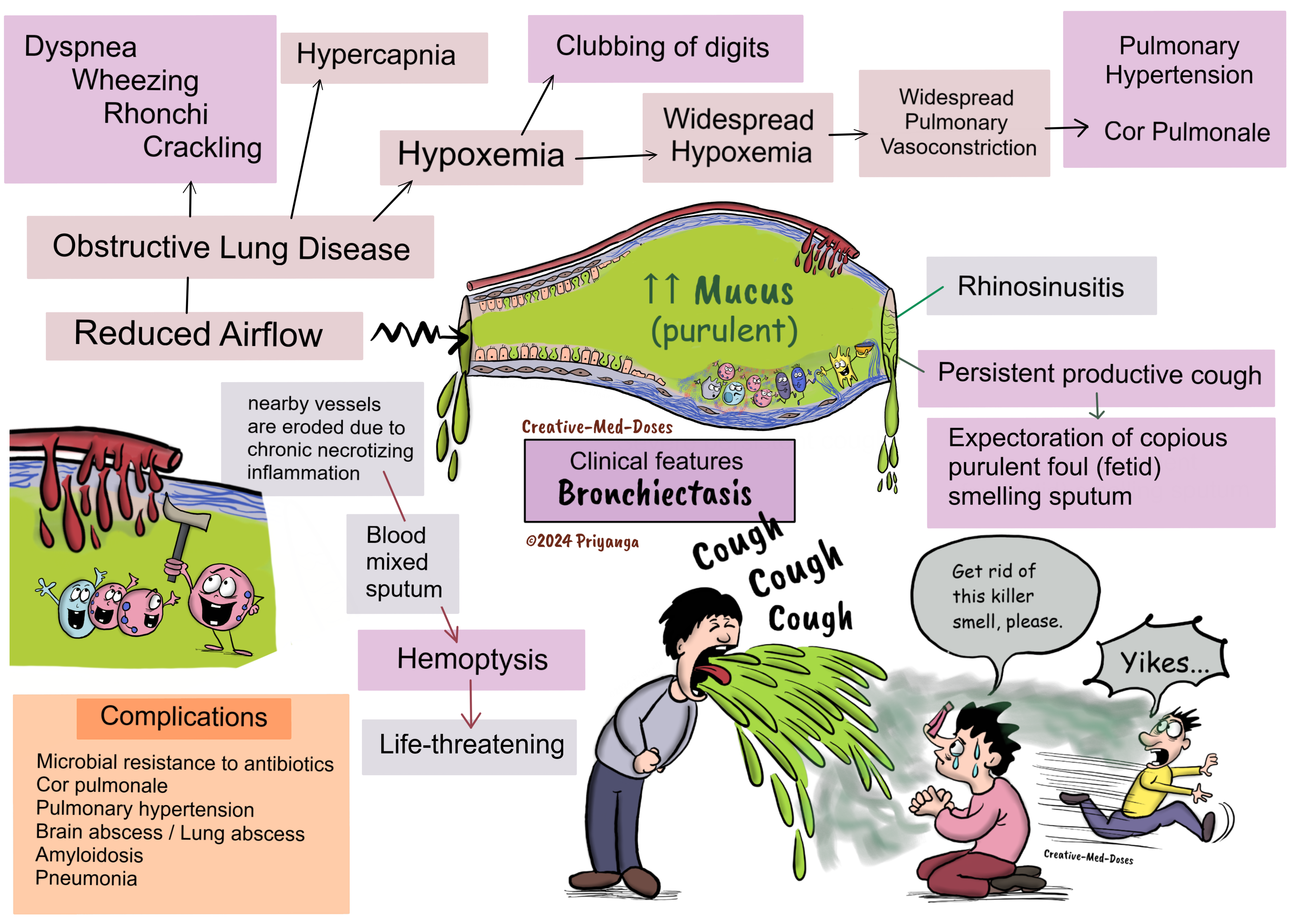
Clinical features
- Persistent productive cough
- Expectoration of copious purulent foul (fetid) smelling sputum
- Tenacious sputum
- Acute exacerbation is associated with sputum changes (increased purulence and volume)
- Hemoptysis (when nearby vessels erode due to chronic necrotizing inflammation)
- Wheezing and crackling on auscultation
- Clubbing of digits due to chronic hypoxemia.
....
....
Diagnosis
Based on clinical presentation and consistent radiological findings.
Chest X-ray - Shows tram tracks sign (thickened bronchial wall)
High-Resolution Computed Tomography (HRCT)- Imaging modality of choice
- Tram track sign- Bronchial wall thickening (parallel tram lines)
- Tree bud appearance – Dilated and thickened bronchial wall with intraluminal inspissated mucus, pus, and fluid resembling a budding tree.
- Signet ring sign- In bronchiectasis, a cross-sectional area of the airway is at least 1.5 times that of the adjacent vessel, and it appears like a signet ring. The bronchus and artery diameter should be the same size, but in bronchiectasis, the dilated bronchi diameter is more than 1.5 times that of the adjacent artery. It gives a signet ring appearance.
- Lack of bronchial tapering (the presence of tubular structures within 1 cm from the pleural surface)
- Cystic dilation of bronchi
Bronchoscopy is done to rule out foreign body or mass causing airway obstruction, especially in cases with focal bronchiectasis.
Pulmonary function testing for functional assessment of the patients – It can be an obstructive, restrictive, or normal pattern.
Treatment
Treat underlying cause – remove the tumor (obstruction) and treat infection.
Controle infection – Antibiotics
Minimize risk of repeated infection
- Antibiotics
- Vaccination
Increased clearance of secretion by
- Adequate hydration
- Mucolytic administration - mucolytic dornase (DNase) (frequently used in cystic fibrosis)
- Chest Physiotherapy
- Postural drainage
- Mechanical chest percussion - Hand clapping on the chest or by high-frequency chest wall oscillation vest.
Bronchodilators
Anti-inflammatory treatment - Glucocorticoids (Oral/Systemic) in cases of -
- ABPA (allergic bronchopulmonary aspergillosis)
- Autoimmune conditions (Rheumatoid arthritis or Sjogren syndrome)
Surgery
Usually considered in refractory cases
- Lobectomy or segmentectomy in localized lung disease
- Lung transplantation in severe cases
Complications
- Microbial resistance to antibiotics because of repeated use in treating recurrent infections.
- Life-threatening hemoptysis – chronic recurrent infections and inflammation may erode nearby supplying vessels, leading to bleeding in the bronchial lumen, consequently causing hemoptysis. Bronchial artery angiography with embolization is the treatment of choice in hemoptysis.
- Cor pulmonale and pulmonary hypertension
- Brain abscess / Lung abscess
- Amyloidosis
- Pneumonia
Prevention
- Vaccination of COPD patients with influenza and pneumococcal vaccines decreases the risk of recurrent infections.
- Gamma globulin for immunoglobulin-deficient patients reduces the risk of recurrent infections.