Acute Respiratory Distress Syndrome (ARDS)
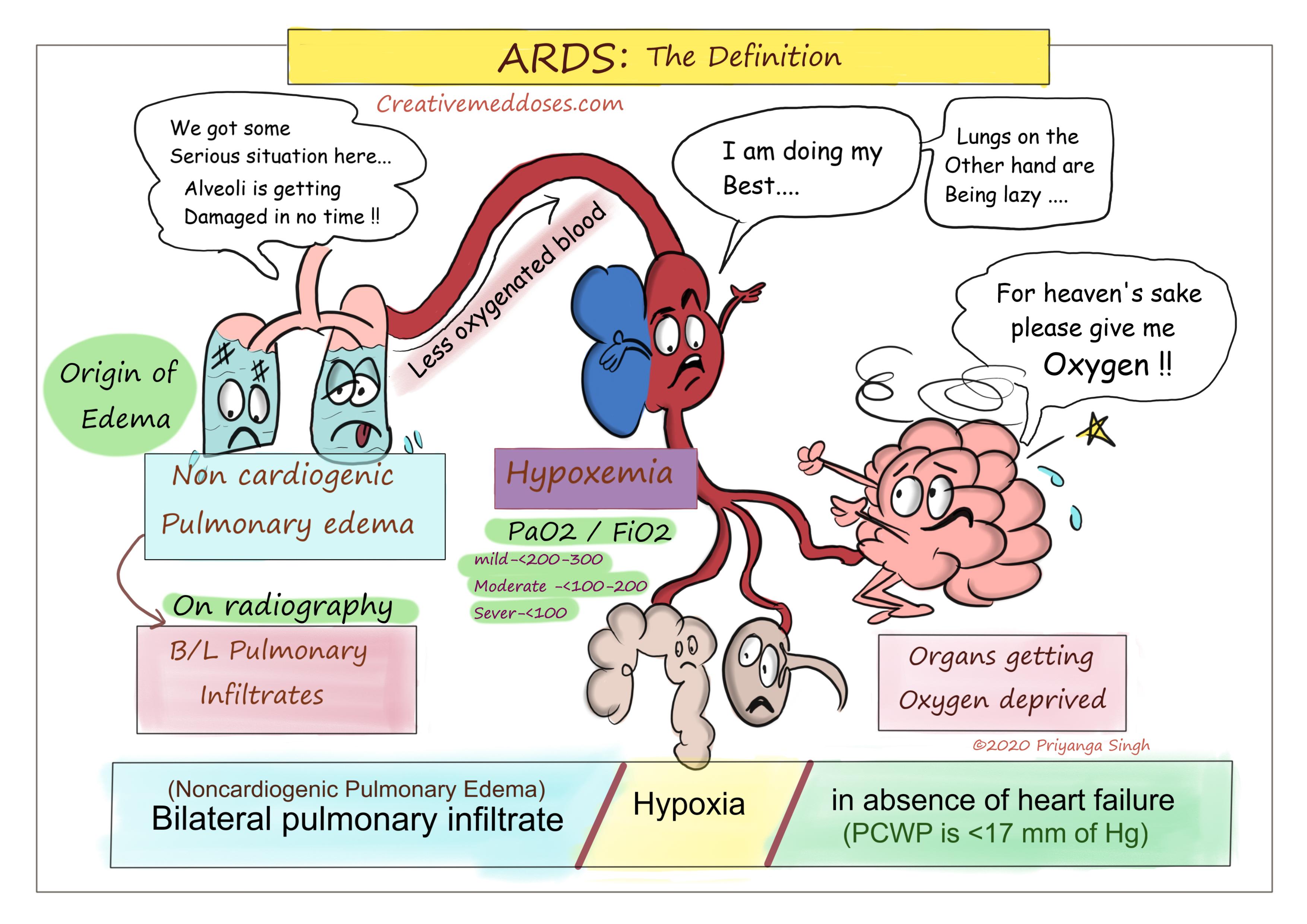
Acute Respiratory Distress Syndrome is a form of non-cardiogenic pulmonary edema, due to diffuse alveolar injury. This diffuse alveolar damage occurs secondary to an inflammatory process. The initiative of inflammation can be Direct injury to the Lung or indirect injury by systemic causes.
According to Berlin criteria: ARDS is defined by timing (within 1 week of clinical insult or onset of respiratory symptoms); radiographic changes (bilateral opacities not fully explained by effusions, consolidation, or atelectasis); origin of edema (not fully explained by cardiac failure or fluid overload); and severity based on the PaO2/FiO2 ratio on 5 cm of continuous positive airway pressure (CPAP). The 3 categories are mild (PaO2/FiO2 200-300), moderate (PaO2/FiO2 100-200), and severe (PaO2/FiO2 ≤100).
...
...
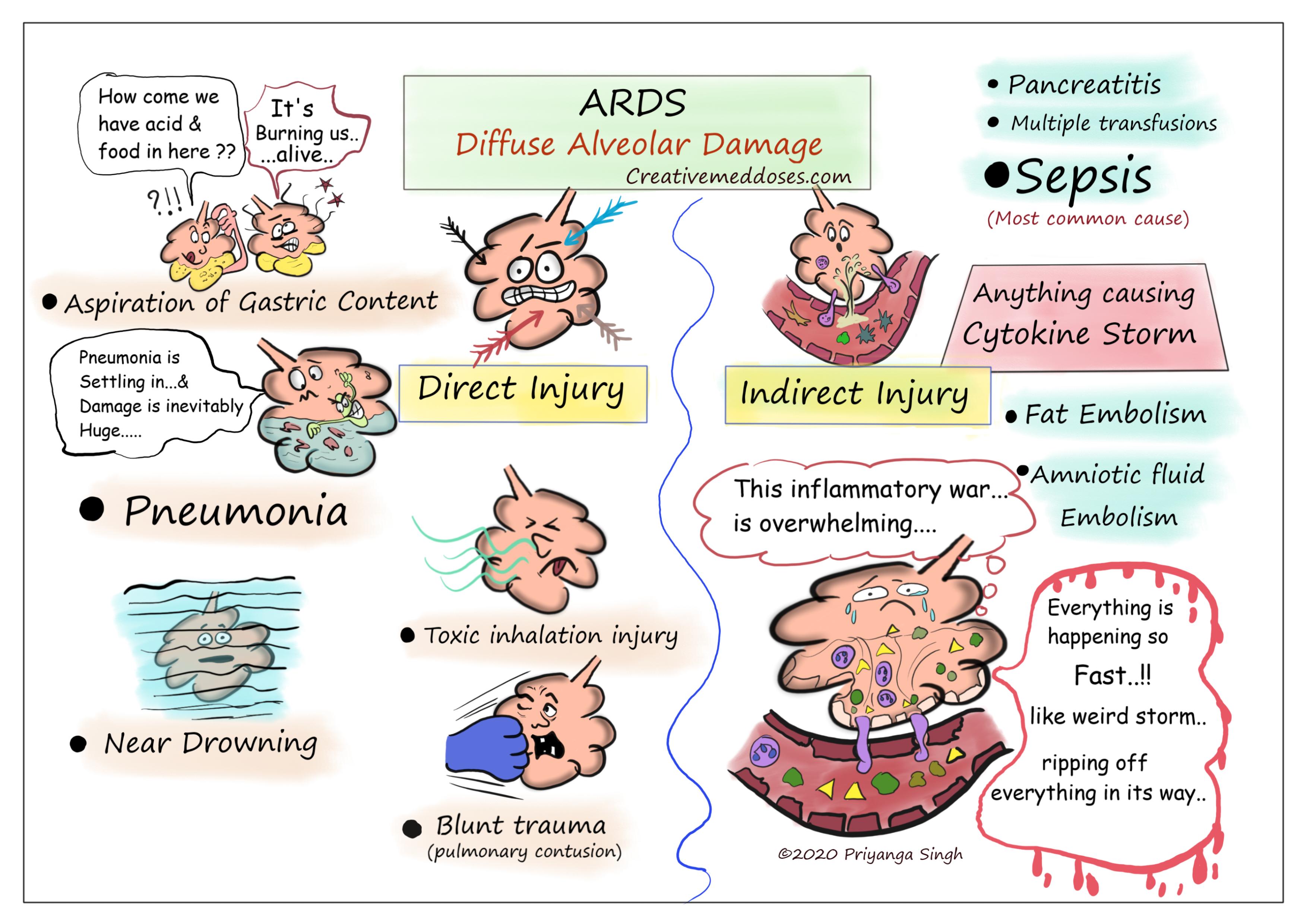
ETIOLOGY
Most cases are attributed to Pneumonia and Sepsis (40-60%).
Clinical Disorders Commonly Associated with ARDS can be of two types-
Direct Lung Injury
- Pneumonia
- Aspiration of gastric contents
- Pulmonary contusion
- Near-drowning
- Toxic inhalation injury
Indirect Lung Injury
- Sepsis
- Long bone fracture (fat embolism)
- Amniotic Embolism
- Multiple transfusions
- Drug overdose
- Pancreatitis
...
...
Pathogenesis
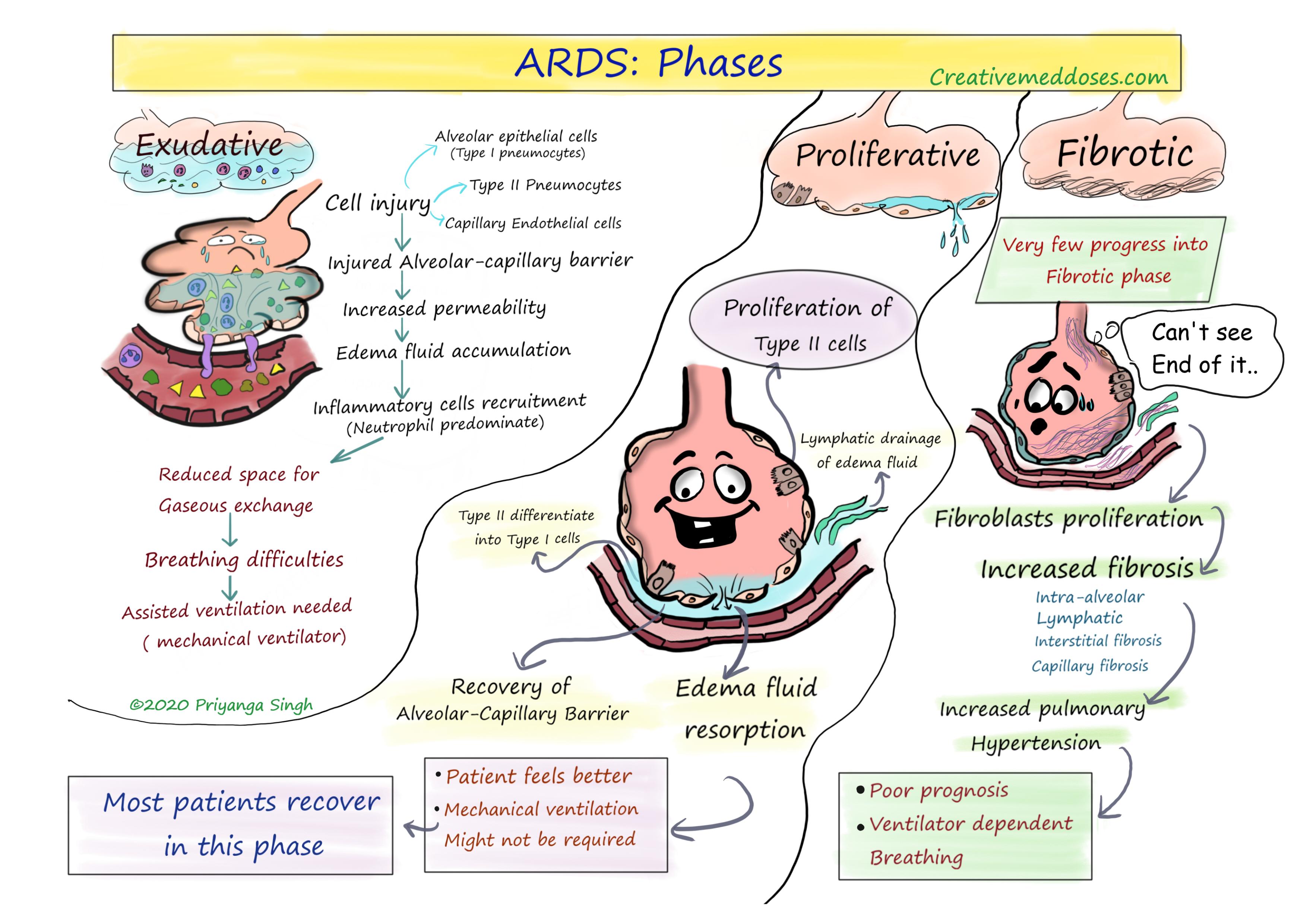
ARDS has three phases—exudative, proliferative, and fibrotic. All of them have characteristic clinical and pathologic features-
Exudative Phase
In this phase, alveolar capillary endothelial cells and type I pneumocytes (alveolar epithelial cells) are injured, and tight alveolar barrier is damaged giving away the entry to fluid and macromolecules. The protein rich edema fluid accumulates in the interstitial and alveolar spaces. Pro-inflammatory cytokines are increased in this acute phase, leading to the recruitment of leukocytes (especially neutrophils) into the pulmonary interstitium and alveoli. There is plasma proteins aggregation in air spaces with cellular debris and dysfunctional pulmonary surfactant to form hyaline membrane whorls. Alveolar edema predominantly involves dependent portions of the lung with diminished aeration. Collapse of large sections of dependent lung can contribute to decreased lung compliance. It causes intrapulmonary shunting and hypoxemia develop and the work of breathing increases, leading to dyspnea.
The exudative phase encompasses the first 7 days of illness after exposure to a precipitating ARDS risk factor. Tachypnea and increased work of breathing result frequently in respiratory fatigue and ultimately in respiratory failure.
Proliferative Phase
This phase of ARDS usually lasts from day 7 to day 21. Most patients recover rapidly and are liberated from mechanical ventilation during this phase. Despite this improvement, many patients still experience dyspnea, tachypnea, and hypoxemia. Histologically, the first signs of resolution are often evident in this phase, with the initiation of lung repair, the organization of alveolar exudates, and a shift from neutrophil- to lymphocyte-predominant pulmonary infiltrates.
As part of the reparative process, type II pneumocytes proliferate along alveolar basement membranes. These specialized epithelial cells synthesize new pulmonary surfactant and differentiate into type I pneumocytes.
Fibrotic Phase
Most patients with ARDS recover lung function within 3–4 weeks, very few progresses into fibrotic phase that may require long-term support on mechanical ventilators and/or supplemental oxygen. There is extensive alveolar-duct and interstitial fibrosis. Marked disruption of acinar architecture leads to emphysema-like changes, with large bullae.
Intimal fibroproliferation in the pulmonary microcirculation causes progressive vascular occlusion and pulmonary hypertension. The physiologic consequences include an increased risk of pneumothorax, reductions in lung compliance, and increased pulmonary dead space.
...
...
Diagnostic workup
Arterial blood gas
- severe hypoxemia on pulse oximetry and ABG
Radiology
- Bilateral alveolar infiltrates on Chest X ray
- ground glass opacities and consolidations on chest CT
Histology
- diffuse alveolar damage
- protein-rich leakage (exudate) forming an intra-alveolar hyaline membrane
Treatment
Treatment of underlying cause
Mechanical ventilation with low tidal volume (4-6 mL/kg ideal body weight) to prevent VALI (ventilator induced lung injury)
Using PEEP (positive end-expiratory pressure) is helpful in reducing lung injury related to airway collapse at end-expiration
- PEEP recruits collapsed alveoli
- It increases FRC and decreases shunting
Subscribe new series “medRational” on youtube for bites of med doses 😎🥰 click here https://www.youtube.com/channel/UCum2ipWFIH68Xt3houEkyKA
Revision for today https://creativemeddoses.com/topics-list/environmental-enteropathy-pathogenesis/